Brucellosis or Undulant fever
Brucellosis of domestic animals, also known as undulant fever, abortion disease, contagious abortion, infectious abortion or Baug’s disease has long been recognised as a major infectious disease of livestock. It is of great economic importance for the agricultural industry but can also be harmful to humans as man can acquire the disease from infected animals. The disease has been partly managed using antibiotics, vaccines and prevention plans. (3)
A zoonotic parasite
A bioweapon
Prevention and cure
The Bison cull
A zoonotic parasite
Undulant fever first came to the attention of British medical officers in the 1850s in Malta and Jeffrey Allan Marston described his own case of the disease in 1861. The bacteria responsible were isolated in 1897. (7, 8) Today, half a million people are infected with this disease each year outside the US.
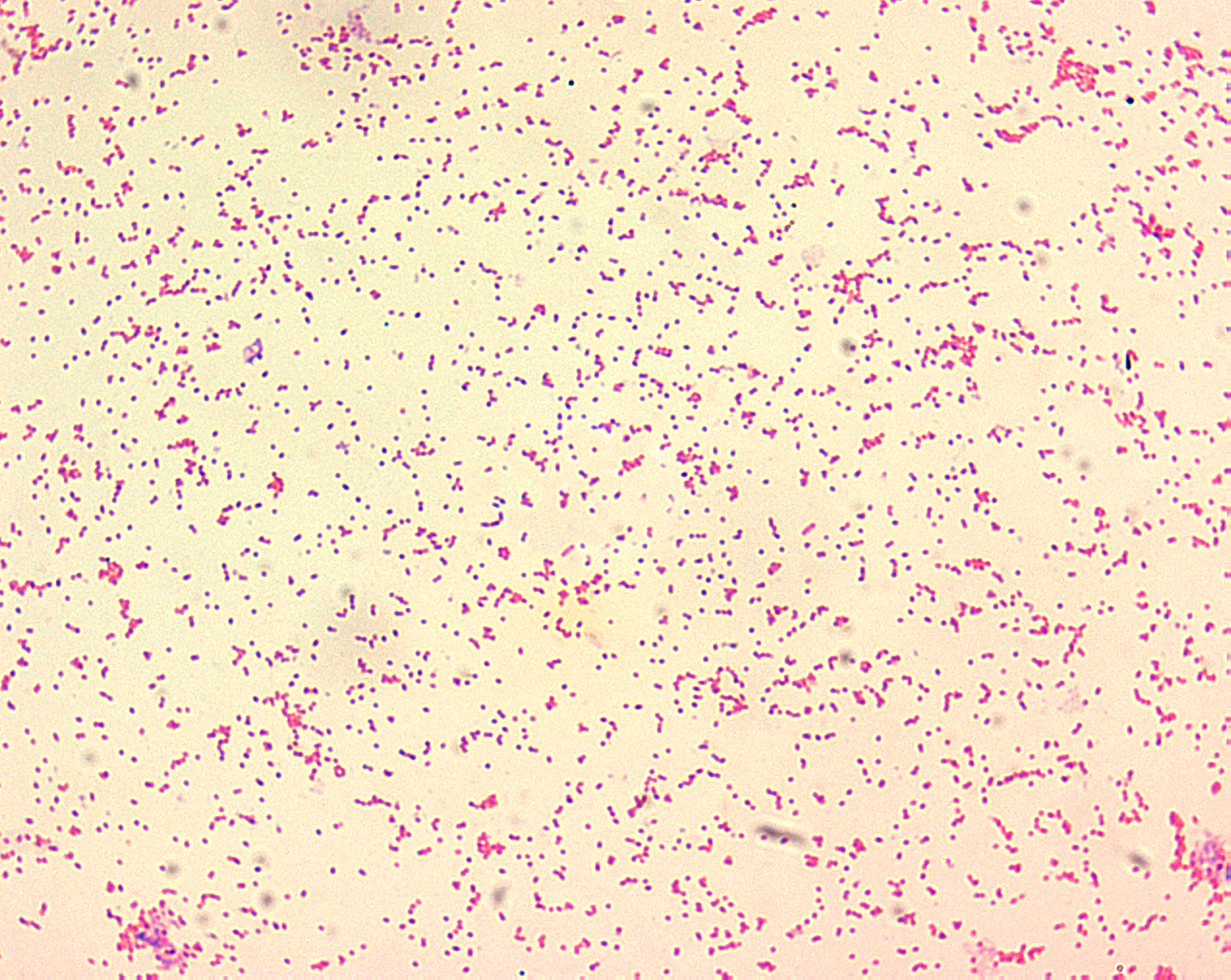
Brucellosis is an infectious disease caused by the gram negative bacteria Brucella. The bacteria act as a facultative intracellular parasite causing chronic disease which usually persists for life. Brucellosis bacteria are engulfed by white blood cells and hide and multiply inside the endoplasmic reticulum (ER) compartment of the cells. Normally a white blood cell would kill a bacterium, but because they reside inside the ER, the white blood cell cannot response to the invaders. The bacteria are transported throughout the body by the white blood cells. (5)
Symptoms include rising and falling fever, sweats, malaise, feeling of weakness, anorexia, headaches and muscle and back pain in humans. The disease can be more or less severe, three forms of the disease exist: the acute form, undulant form, and the chronic form. (1)
The disease is a zoonosis, meaning it can cross between different species. Cows, goat, sheep, pigs, caribou, bison, camels, elk, cetaceans, seals and dogs, have all been shown to be affected by different bacteria of the Brucella family. (9, 10, 11). These infections usually impact on fertility and can often lead to abortions. (4)
The disease is transmitted to humans through contaminated and untreated milk and by direct contact with the infected animals, dead or alive.
Millions of people are at risk for the disease, especially in developing countries, where the infection in animals has not been brought under control, where heat treatment are not routinely applied and where food consumption of raw milk and poor hygienic conditions favour human infections. (1)
A bioweapon
Brucella species were weaponized by several countries in the mid-20th century. In 1954, B. suis – the pig brucellosis - became the first weaponized agent by the US as brucella species survive well in aerosols. However, the weaponized brucella were not very effective and had a low mortality rate. (12)
Prevention and cure
The mortality rate of the disease is quite low at around 2% and recent advances in antibiotics and surgery have been successful at preventing death by endocarditis. (13) Antibiotics are effective against Brucella, but because the bacteria are located within the cells, several different antibiotics are required. (1)
A vaccine exists for cattle but unfortunately, there is currently no effective vaccine for humans (13). However, work is underway to understand how the Brucellosis bacteria reach the ER in the white blood cells and what leads the bacteria to exit infected cells and spread further. This might help develop medication that could block the infection process. Additionally, if research leads to a better understanding of how Brucellosis works in our bodies, it might help with dealing with other diseases that hijack the immune system such as tuberculosis (5).
Brucellosis can be prevented in people by controlling and eliminating the disease in animals; by vaccination or other control methods such as testing herds and killing the infected animals; and by avoiding the consumption of raw milk. Proper heat treatments of milk are important to destroy the bacteria. (1, 13)
In the US, dairy herds are tested at least once a year and contaminated animals are often killed to avoid disease spread. Vets are required to vaccinate all young stock thereby decreasing the risk of zoonotic and inter-species transmission. (14)
The Bison cull
Wild bison and elk in the Yellowstone Area in the US are the last remaining reservoir of Brucella bacteria that can infect cattle. Recent transmissions from the wild animals to livestock have been recorded and might affect the industry, consequently some people wish to eliminate the threat from the area. However, this poses a challenge, as many viewpoints exist on how to manage disease in wildlife.
Roughly half of the Yellowstone’s bison have been exposed to the disease, probably originally brought to the park by the cattle that once grazed there.
Every year, the few bison that stray from the park area are culled to avoid the spread of the disease to livestock. This winter, some 900 bison were culled, about one fifth of the herd – the largest cull in seven years. This push to cull the fragile herd of the last pure-bred remaining bison is tied to a long-standing management plan hammered out among federal and state wildlife and agricultural agencies that sets the target population at 3000 to 3500.
This cull might also be a way the livestock industry eliminates competition and maintains control of grazing lands surrounding the park. Ironically, there has never been a proven case of wild bison transmitting brucellosis to livestock. (6)
The US Interior Department is considering a new plan that would potentially allow new, disease-free bison herds to repopulate much of the land they used to roam across, The plan is based on the idea that the government can move various herds to external sites where they would be quarantined for some years in an attempt to keep the disease from spreading. If the disease can be successfully left behind, the healthy buffalo would be taken to other parts of the west US where they could establish new populations. (2)
References
- http://www.medicinenet.com/script/main/art.asp?articlekey=9306
- http://www.doi.gov/news/pressreleases/interior-department-releases-report-on-bison-management-reaffirming-commitment-to-work-with-states-tribes-and-other-partners.cfm
- http://jama.jamanetwork.com/article.aspx?articleid=248872
- http://cattletoday.info/brucellosis.htm
- http://cahnrs.wsu.edu/blog/2013/11/undulant-fever-in-cattle-and-people/
- http://www.reuters.com/article/2014/09/17/us-usa-bison-yellowstone-idUSKBN0HC01F20140917
- Wilkinson, Lise (1993). ""Brucellosis"". In Kiple, Kenneth F. (ed.). The Cambridge World History of Human Disease. Cambridge University Press)
- Brucellosis named after Sir David Bruce at Who Named It?
- Radostits, O.M., C.C. Gay, D.C. Blood, and K.W. Hinchcliff. 2000. Veterinary Medicine, A textbook of the Diseases of Cattle, Sheep, Pigs, Goats and Horses. Harcourt Publishers Limited, London, pp. 867–882
- Ettinger, Stephen J; Feldman, Edward C. (1995). Textbook of Veterinary Internal Medicine(4th ed.). W.B. Saunders Company. ISBN 0-7216-4679-4
- Guzman-Verri, Caterina , Rocio Gonzalez-Barrientos, Gabriela Hernandez-Mora, Juan-Alberto Morales, Elias Baquero-Calvo, Esteban Chaves-Olarte, and Edgardo Moreno. Brucella ceti and Brucellosis in Cetaceans. : US National Institutes of Health , 2012
- Woods, Lt Col Jon B. (ed.) (April 2005). USAMRIID’s Medical Management of Biological Casualties Handbook (PDF) (6th ed.). Fort Detrick, Maryland: U.S. Army Medical Institute of Infectious Diseases. p. 53
- Yagupsky, Pablo; Baron, Ellen Jo (August 2005). "Laboratory Exposures to Brucellae and Implications for Bioterrorism". Emerging Infectious Diseases 11 (8): 1180–1185.doi:10.3201/eid1108.041197
- ermont Beef Producers. "How important is calfhood vaccination?"
Last edited: 27 May 2015 14:57

