BSE & CJD
 CJD – Creutzfeldt-Jakob disease – is a fatal brain disease. It used to be very rare, affecting about 30 people a year in the UK. Most were elderly. More recently, the rate has increased owing to variant CJD (vCJD) transmitted from cattle affected with bovine spongiform encephalopathy. Most vCJD patients are young. Cases of vCJD peaked in 2000, when 28 deaths were reported. Since then the trend has been generally downward, with 17 cases in 2002 and 9 in 2004.
CJD – Creutzfeldt-Jakob disease – is a fatal brain disease. It used to be very rare, affecting about 30 people a year in the UK. Most were elderly. More recently, the rate has increased owing to variant CJD (vCJD) transmitted from cattle affected with bovine spongiform encephalopathy. Most vCJD patients are young. Cases of vCJD peaked in 2000, when 28 deaths were reported. Since then the trend has been generally downward, with 17 cases in 2002 and 9 in 2004.
The role of animal research
Susceptibility
Transmission
Vaccine Research
The role of animal research
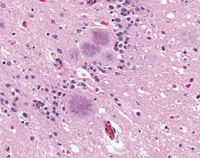
Animal models are crucial in understanding the transmissible spongiform encephalopathies (TSEs) - scrapie in sheep, BSE in cattle, and CJD in humans. These diseases are caused by abnormal versions of prion proteins in the brain. These are not broken down and they also convert normal prions to the abnormal version. The resulting accumulation of abnormal prions and loss of normal prion function are thought to cause brain damage.
Key areas of current research involving animals (mainly mice) relate to early diagnosis of these conditions, study of how the diseases progress, how they are transmitted within and between species, establishing safety limits, and developing therapies.
The disease has a long latent period before it causes symptoms, which means that someone can pass it on unknowingly. Circumstantial evidence has long suggested that it was transmitted both orally and intravenously but this was not proved until 2004, in research on monkeysANCHOR. Shortly afterwards a method was developed, using hamsters, that enabled the disease-causing prion protein to be recognised in the muscles of symptoms-free animals incubating the diseaseANCHOR.
The similarity of symptoms and brain pathology in vCJD patients and in animals with BSEANCHOR ANCHOR, suggested a link between these two diseases. Further evidence came from studies using mice. Mice injected with prions from BSE infected cows or with prions from patients with vCJD showed the same pattern of brain damageANCHOR. This led to the conclusion that the disease known as vCJD was a human form of BSE.
Susceptibility
Scientists have discovered, using mice with an underdeveloped immune system, that a certain type of immune system cell is required for infectious prion diseases to develop. Drugs that target these cells may provide a treatmentANCHOR. Three areas on the mouse chromosome have been linked to increased susceptibility and and the same is true of humansANCHOR.
Transmission
In studies on transmission of BSE, mice have been genetically engineered to react to CJDANCHOR. The studies suggested that there is some form of species barrier. However, such species barriers have been called into question following researchANCHOR that shows that abnormal prions can be transmitted from hamsters to mice without the mice showing any symptoms. Tests on sheep have also shown that before an animal shows obvious signs of disease it is capable of transmitting BSE-like disease to another animalANCHOR. Similarly, studies in lemur monkeysANCHOR showed that they were easily infected orally with BSE: five months after being fed with infected cattle brain, the infection had spread to their tonsils and other tissues although the animals showed no outward signs of disease.
It has been found that vCJD patients all have two copies of the MM gene at codon 129. This is found in 40% of the population. It seems that people with one or no copies do not develop the disease, even if infected. However, studies in mice suggest that these individuals can carry the infection, meaning there may be unrecognised cases in the population. Affected mice with the disease did not show any outward symptoms of disease, but this might be because they have a short lifespanANCHOR.
BSE had been thought to occur only in the lymphoid (immune) and nervous systems of infected animals. This belief has underpinned the strategy used to eradicate BSE. But scientists studying mice now report that the prions can travel to other organs as well. This happens when there is an inflammatory response to illness or infection. We may yet need to re-think our prevention strategyANCHOR.
Vaccine Research
Synthetic compounds that prevent normal prions from converting to the abnormal, infectious type, have been developed. They stop the formation in the test tube of infective prions and substantially decrease the infectivity of scrapie in miceANCHOR ANCHOR, suggesting they might have the same effect in patients with vCJD. The work has led to a vaccine that delays the onset of a mad-cow-like disease in mice. Though preliminary, the results could lead to vaccines against scrapie in sheep, BSE in cattle and vCJD in humansANCHOR.
When mice are injected with antibodies 30 days into the disease, before symptoms occur, the diseases doesn't develop, even though the prions are multiplying furiously. It probably stops the prions from folding into the disease-causing, misshapen form. Before they can be used clinically the antibodies will have to be 'humanised' but this should not be a problem. The antibodies will have to be injected into the brainANCHOR, but such injections are feasible.
In mice injected with scrapie, disease onset is delayed when modified normal prions are injected. It might be possible to harness this effect in a vaccineANCHOR. In a strange twist to this, scientists studying BSE in mice found that misshapen prions seem unable to cause disease without the help of their normal brethren: the disease process goes into reverse when the production of normal prions is stoppedANCHOR. Removing one part of the immune system delays the onset of symptoms in mice. Treatment with cobra venom factor (CVF), which reduces a molecule called C3, delayed symptoms of scrapie infection in miceANCHOR. Mice with scrapie live 38% longer with compounds called CpG oligonucelotides, which are known to be safe in humansANCHOR.
References
- Herzog C, Sales N, Etchegaray N et al (2004) Tissue distribution of bovine spongiform encephaloppathy agent in primates after intravenous or oral infection. Lancet 363, 422.
- Thomzig A, Schulz-Schaeffer W, Kratzel C et al (2004) Preclinical deposition of pathological prion protein PrPSc in muscles of hamsters orally exposed to scrapie. J Clin Invest 113, 1465.
- Collinge J, Sidle KCL, Meads J, Ironside J, (1996) Molecular analysis of prion strain variation and the aetiology of 'new variant' CJD Nature 383, 685.
- Bruce ME, Will RG, Ironside JW, McConnell I, Drummond D, Suttie A, McCardle L, Chree A, Hope J, Birkett C, Cousens S, Fraser H, Bostock CJ (1997) Transmissions to mice indicate that 'new variant' CJD is caused by the BSE agent Nature 389, 498.
- Scott M, Will R, Ironside J et al (1999) Compelling transgenic evidence for transmission of bovine spongiform encephalopathy prions to humans Proc Nat Acad Sci 96, 15137.
- Brown KL, Stewart K, Ritchie DL et al (1999) Scrapie replication in lymphoid tissues depends on prion protein-expressing follicular dendritic cells Nature Med 5, 1308.
- Lloyd SE, Onwuazor ON, Beck JA et al (2001) Identification of multiple quantitative trait loci linked to prion disease incubation period in mice Proc Nat Acad Sci, 98, 6279.
- Hill AF, Desbruslais M, Joiner S, Sidle KCL, Gowland I, Collinge J, Doey LJ, Lantos P (1997) The same prion strain causes vCJD and BSE Nature 389, 448.
- Hill AF, Joiner S, Linehan J, Debruslais M, Lantos PL, Collinge J (2000) Species-barrier-independent prion replication in apparently resistant species. Proc Nat Acad Sci, 97, 10248.
- Houston F, Foster JD, Chong A, Hunter N, Bostock CJ (2000) Transmission of BSE by blood transfusion in sheep Lancet, 356, 999.
- Bons N, Mestre-Frances N, Belli P, Cathala F, Gajdusek DC, and Brown P (1999) Natural and experimental oral infection of nonhuman primates by bovine spongiform encephalopathy agents Proc Nat Acad Sci 96, 4046.
- Wadsworth JDF, Asante EA, Desbruslais M et al (2004) Human prion protein with valine 129 prevents expression of variant CJD phenotype. Science 306, 1793
- Heikenwalder M, Zeller N, Seeger H et al (2005) Chronic lymphocytic inflammation specifies the organ tropism of prions. Science 307, 1107
- Soto C, Kascsak R, Saborio G et al (2000) Reversion of prion protein conformational changes by synthetic beta-sheet breaker peptides Lancet 355, 192.
- Priola SA, Raines A, Caughey WS (2000) Prophyrin and phthalocyanine antiscrapie compounds Science 287, 1503.
- Sigurdsson EM, David R. DR, Daniels M et al Immunization delays the onset of prion disease in mice Am J Pathol 2002 161, 13-17.
- White AR, Enever P, Tayebi M et al (2003) Monoclonal antibodies inhibit prion replication and delay the development of prion disease. Nature 422, 80.
- Meier P, Genoud N, Prinz M et al (2003) Soluble dimeric prion protein binds PrPSc in vivo and antagonizes prion disease. Cell 113, 49.
- Solforosi L, Criado JR, McGavern DB et al (2004) Cross-linking cellular prion protein triggers neuronal apoptosis in vivo. Science 303, 1514.
- Mabbott NA, Bruce ME, Botto M, Walport MJ & Pepys MB (2001) Temporary depletion of complement component C3 or genetic deficiency of C1q significantly delays onset of scrapie Nature Medicine 7, 485.
- Sethi S, Lipford G, Wagner H, Kretzschar H. (2002) Postexposure prophylaxis against prion disease with a stimulator of innate immunity. Lancet 360, 229.
Last edited: 27 August 2014 05:57
