Influenza
Influenza is a common viral respiratory disease, which is easily passed from between people via small droplets when an infected person coughs or sneezes. Most people recover from 'flu in a couple of weeks without the need for treatment, but in some circumstances the virus may lead to pneumonia or even death. In 1918 a world-wide pandemic of Spanish Flu killed between 40-50 million people - more than the First World War1. Today, annual influenza epidemics cause about 250,000 to 500, 000 deaths worldwide, and are monitored by the World Influenza Centre. The recent outbreak of H1N1 flu virus has reached pandemic level, and precautions to limit its damage are being taken around the world.
The influenza virus
The ferret model
The influenza vaccine
Flu vaccine production
Antivirals
Avian flu
H1N1 swine flu virus
The Influenza virus
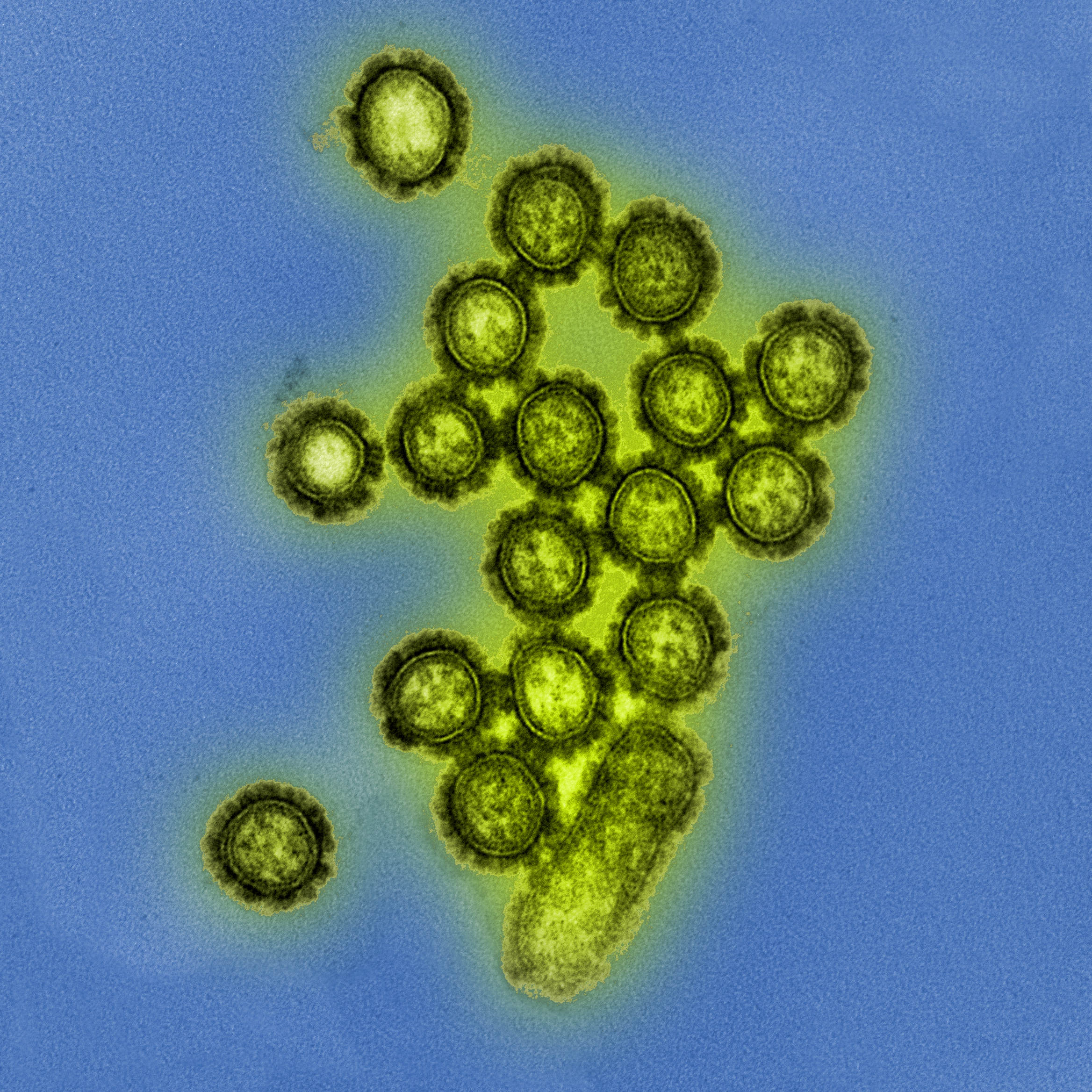
There are three types of influenza virus, A, B and C. Influenza A viruses are found in humans and animals, whereas B and C strains infect only humans. Influenza A virus produce two surface proteins (usually shown as projections from the virus surface), haemagglutinin (H) and neuraminidase (N), which are used to classify the virus into subtypes – H1N1 for example. There are 15 variations of the HA protein, and nine variations of the NA protein. These two surface proteins may change over time and this affects our ability to fight the virus.
Our bodies launch an immune response when infected with influenza, producing antibodies which circulate in the blood and neutralise the virus. If we encounter the same virus again, while the antibodies are still present, we are protected and should not develop an infection. However, these antibodies will not protect individuals against an influenza virus if the surface proteins have undergone a significant change since the previous infection.
A single cell can be infected by two strains of influenza at the same time. When this happens the strains can swap genes, leading to the production of completely new viruses. This process, known as antigentic shift, occurs in influenza A strains which infect both animals and humans, enabling animal strains of 'flu can become infectious to other species. For example, a pig may become simultaneously infected with human and avian strains of flu. The genes from each strain mix inside the pig’s cells to produce a new variety of influenza which is also infectious to humans. Because the human immune system has difficulty recognizing the new virus, with its combination of surface proteins from both the avian and human flu strains, it may be highly dangerous. It is this phenomenon of antigenic shift that causes nation-wide epidemics and world-wide pandemics.
The Ferret Model
The ferret is the best model for studying influenza in humans. Types A and B of human influenza naturally infect the ferret, and the infection closely resembles that in humans, with similar clinical indicators, pathology and immunity.
Ferrets are used to study age-related susceptibility to influenza infection and have also played an important role in understanding the development process of typical influenza infections. They have helped to understand transmission and reassortant variants of the virus. Ferrets have also been used to study Reynes syndrome, and the resistance of 'flu viruses to many antiviral drugs.
In vaccine development ferret models are used to produce anti-sera to past infections. This anti-sera is used to induce influenza in naïve ferrets so that it can be compared with a natural infection, allowing scientists to differentiate between different antigenic strains. When strains of influenza virus that are different to the previous season’s viruses are found ferrets are used to produce anti-sera to the new strains so that vaccines to the newest strains of 'flu are available.
Recently, ferrets were used to establish that the virulence of the new H1N1 swine related virus is greater than normal seasonal H1N1. Ferrets are also used to test the virulence of recombinant inactivated viruses for vaccine development, making sure that they are completely inactivated and don’t induce an influenza infection. Anti-sera for measuring the potency of a vaccine, to establish the required dose, are made in sheep.
The Influenza Vaccine
Influenza vaccines have been available for over 50 years. They are usually tri-valent - containing three different inactivated virus strains. The vaccine causes an immune response, enablling the immune system to recognise the virus in the future, but does not lead to a full influenza infection.
Because the virus is constantly changing through antigenic drifts and shifts, the vaccine needs to be adapted to changes regularly to protect against those currently in circulation. The Global Influenza Surveillance Network of the World Health Organisation (WHO) monitors these changes and recommends the strains to be included into the vaccine for the coming season.
Vaccine Production
Traditionally, influenza vaccines are produced in fertilised chicken eggs. Eleven days after fertilisation an influenza virus is injected into the eggs and infects the embryo, where it multiplies. After several days of incubation, machines open the eggs to harvest the virus, which is then purified and chemically inactivated.
The overall capacity of this production process is limited as one to two eggs are needed to produce only one dose of vaccine and the whole process takes around six months. The process is not suited to emergencies, as it is impractical to keep millions of eleven day old eggs on standby and the length of time to produce a vaccine is prohibitive.
Alternatively, vaccines can be produced in tissue culture, which involves growing viruses in bioreactors containing large numbers of cells. The infected cells are harvested, and the virus is purified and inactivated. In an emergency situation this method is better than the egg based process because production can be rapidly expanded and scaled up. It does not carry a risk of allergies to the egg albumin or problems from impurities in the eggs which are associated with the traditional method. However, the cost to maintain sufficient bioreactor capacity for emergency use is high, and yields may be slightly lower.
Today’s flu vaccines need to be adapted each year to new virus strains, but researchers hope that in the future a vaccine will be developed that will provide immunity against all strains of influenza. New research has brought this goal a step closer.
In early 2009, scientists found a family of lab-made proteins, called monoclonal antibodies, that neutralize a broad range of influenza A viruses, including the avian virus H5N1, the 1918 pandemic virus and seasonal H1N1 viruses. Because large quantities of monoclonal antibodies can be made relatively quickly, after further tests these proteins could be used in combination with antiviral drugs to prevent or treat 'flu in an outbreak or pandemic.
The antibodies bind to a genetically stable region on the neck of the HA protein, which prevents the virus changing shape. The protien is essential to the virus, and without its capacity for structural change it is unable to fuse with, and enter a host cell. The scientists found no viruses that mutated to exclude the antibodies, so this technique may work for all 'flu viruses. These stable pockets which do not mutate may be from evolutionary constraints that enable virus-cell fusion – without them the virus would not be able to enter host cells.
This research could aid vaccine development, as current vaccines do not readily generate antibodies against this conserved region. Redirecting the body's immune response to this part of the virus could lead to a vaccine that gives life-long immunity. The monoclonal antibodies are about to go into pre-clinical testing in ferrets and the researchers hope to test in clinical trials with human subjects in the next 18 months2.
Antivirals
Vaccine development is only partially effective in controlling influenza epidemics due to the rapid rate of antigenic change in surface proteins. There are also difficulties in generating and manufacturing new vaccines rapidly enough to protect against pandemic virus strains. At the present time antiviral agents are therefore essential to enabling control of influenza.
The first antiviral agents, called amantadine and rimantadine, inhibited viral replication by interfering with an M2 ion channel; a protein that the virus needs to reach the host cell’s nucleus. These drugs are not widely used because of their ineffectiveness against influenza B strains as drug-resistant variants emerged rapidly. This virus developed resistance through mutations in the ion channel protein, preventing the antiviral drug from binding and taking effect.
The development of drugs that block the action of neuraminidase have revolutionised influenza management, as these inhibitors are effective against both A and B strains of the virus. Neuraminidase is an enzyme that is essential for viral replication and infectivity. It is thought to be required for the release of newly produced viral particles from infected cells and aids movement of the virus through the respiratory tract.
The susceptibility of the influenza virus to the first neuraminidase inhibitor, zanamivir (Relenza)3, was tested in-vitro on canine kidney cells and human epithelial cells. The activity of the drug was tested in mice and ferrets, and pre-clinical safety tests were carried out in dogs and rats. The drug then entered clinical evaluations and was tested on human volunteers. These clinical studies showed that early treatment with zanamivir significantly shortens the duration of influenza illness and is an effective prophylaxis. One disadvantage is that it cannot be administered orally and must be applied directly to the respiratory tract by an inhaler.
Oseltamivir (Tamiflu) was the first orally administered neuraminidase inhibitor, and was developed through pre-clinical tests on rats, mice, dogs and ferrets4. Oseltamivir is a prodrug, meaning that it’s metabolised by the body into its active form, which itself has poor bioavailability if taken orally. Like zanamivir, it’s effective against human influenza A and B strains, and functions as a prophylactic. But it has the added advantage of oral administration.
Resistance to oseltamivir has developed through mutations in the neuramindase enzyme and is becoming a problem. The drug mimics the natural substrate (host-cell sialic acid receptors) of neuraminidase, and by developing mutations that prevent the drug binding, but still allow the protein to function, the virus develops resistance. This is less of a problem with zanimivir, because this drug binds neuraminidase in a different way and is not affected by mutations.
Although many oseltamivir-resistant(non-H5N1) viruses that have been studied in animals are not virulent ar particularly infectious strains, some resistant variants have been transmittedamong ferrets, raising concern that such viruses could be transmitted amonghumans. Recent data collected in Japanby the Neuraminidase Inhibitor Susceptibility Network, found 3 of1,200 isolates from ill patients without known exposure to neuraminidaseinhibitors contained resistance mutations, suggesting that theseresistant viruses are transmitted at least at a low level inhumans and are not severely biologically compromised5.
The highest rates of oseltamivir resistance to have been reported were found in Japan during the winter season 2005-06, when 2.2 % of 178 H1N1 isolates were found to be resistant. During the season 2006-7, no resistant H1N1 variants were detected in isolates from Japan or Europe, and less than 1% of U.S. H1N1 isolates showed oseltamivir resistance6.
However, oseltamivir resistance is well-known to emerge in people being treated with the drug. In clinical studies, resistant H1N1 viruses with a particular mutation have been detected in up to 16% of H1N1-infected children treated with oseltamivir7. Typically, the resistant strains have emerged 3 to 6 days after treatment started, but were not detected a few days later. Past studies found little evidence of spread of resistant H1N1 virus to contacts or circulation within the community. However, the oseltamivir-resistant H1N1 viruses observed in 2008 were different in that they are able to transmit from person to person.
Like any successful infectious agent, influenza viruses will mostlikely evolve to evade any single drug. Targeting severalpoints in the viral life cycle simultaneously with differentdrugs will discourage the emergence of virusesthat can resist all drugs at once.
Avian flu
Influenza A viruses occur naturally in wild birds. Although they’re not affected by the infections, humans and domestic birds, such as chickens, are. Of all the viruses that circulate in birds, H5N1 is the greatest concern for human health. This virus has caused the highest number of severe illness and the most deaths. It has crossed the species barrier to infect humans at least three times in recent years.
A far greater concern is that the H5N1 virus will develop the characteristics it needs to start a pandemic. It already has most prerequisites to do this, apart from one – the ability to pass from human to human.
The virus has become common amongst birds in Asia, and new flu strains tend to occur in Asia, Africa and the east. People sometimes live closely with their animals in these regions, and can pick the virus up when it is shed in an infected bird’s saliva and faeces. Millions of chickens and ducks in South East Asia have been slaughtered to prevent the virus spreading from birds to humans.
Recent research suggests that the potential for an avian flu pandemic is greater than previously thought. The study showed that after reassortment with a human virus, an avian flu virus takes relatively few mutations to spread rapidly between mammals5. Scientists created a human-avian hybrid virus, similar to the virus causing the recent swine flu outbreak. They infected ferrets with the virus which then replicated and mutated. The researchers found that after a short time the virus was transmissible between ferrets and spread by respiratory droplets. On comparing the genetic sequences of the mutated virus and the original hybrid virus, the only differences found were five amino acid mutations. Two of which were determined to be solely responsible for supporting respiratory droplet transmission.
The researchers don’t yet know if the mutations they saw are the same that have made H1N1 swine flu transmissible between humans, and will be doing research on the current swine flu strain to study the specific mutations.
H1N1 Swine Flu Virus
Pigs are known to act as a mixing pot for human, avian and swine influenza viruses. Between the 1930’s and 1990’s the most common swine influenza A (H1N1) changed very little. But by the late 1990’s multiple strains and subtypes of triple reassortant swine influenza A viruses (with genomes including combinations of human, avian and swine influenza virus genes) had emerged and became common in North American pig herds.
Until recently there were very few cases of human infection with swine influenza, and only limited, non-sustained, human to human transmission of the virus had been reported. But since the first reports of significant human infection on April 21st 2009, the virus has spread to 79 countries. On June 11th 2009 the WHO declared a pandemic.
The virus responsible is related to the swine influenza A (H1N1) viruses recently circulating in pigs in North America and Europe/Asia. Its genetic makeup is a mixture of genes from viruses found in both these geographical regions; comprising six genes that include haemagglutinin genes, similar to those of the American triple reassortant swine viruses, and two genes encoding the neuraminidase and matrix proteins, similar to those of European and Asian swine viruses. This strain of virus has not previously been recognized in animal or human populations.
These viruses are sensitive to the neuraminidase inhibitor class of anti-viral drugs, oseltamivir and zanamivir, but they are resistant to amantadine and rimantadine. The WHO and its partners are currently monitoring antiviral drug resistance and the spread of the virus. A vaccine is being developed in several laboratories around the world inluding NIMR and CDC.
References
-
World Health Organisation http://www.who.int/csr/disease/influenza/pandemic10things/en/ (accessed 03.07.09)
-
J Sui et al (2009) “Structural and functional bases for broad-spectrum neutralization of avian and human influenza A viruses.” Nature Structural & Molecular Biology, DOI: 10.1038/nsmb.1566 (2009)
-
Elliott, M. (2001) "Zanamivir: From Drug Design to the Clinic" Phil. Trans. R.Soc. London. B 356, 1885 - 189
-
Weixing, L. et al (1998) "Identification of GS 4104 as an Orally Bioavailable Prodrug of the Influenza Virus Neuraminidase Inhibitor GS 4071." Antimicrobial Agents and Chemotherapy Vol42. No3. p647-653
-
World Health Organisation http://www.who.int/csr/disease/influenza/oseltamivir_faqs/en/index.html (accessed 03.07.09)[6] ibid.
-
Moscana, A (2005) “Oseltamivir Resistance — Disabling Our Influenza Defenses.” The New England Journal of Medicine. Volume 353:2633-2636 Number 25
-
Sorrell, E et al (2009) PNAS “Minimal molecular constraints for respiratory droplet transmission of an avian–human H9N2 influenza A virus.” PNAS May 5, 2009 vol. 106 no. 18 7565-7570. doi 10.1073/pnas.0900877106
Last edited: 24 September 2018 16:38
